Nerve compression is a common condition that affects millions of people worldwide, leading to discomfort, pain, and sometimes significant impairment in daily activities. Understanding nerve compression — what causes it, how to recognize its symptoms, and which treatments are most effective — can empower you to seek the right care and improve your quality of life. In this comprehensive guide, we’ll explore the various facets of nerve compression, providing valuable insights to help you manage this condition effectively.
What Is Nerve Compression?
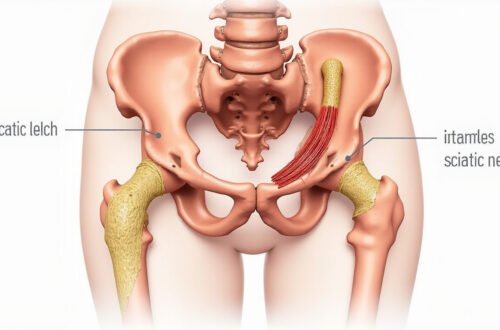
Nerve compression occurs when surrounding tissues—such as bones, muscles, tendons, or cartilage—apply pressure to a nerve. This pressure can disrupt normal nerve function, resulting in pain, numbness, tingling, or weakness in the affected area. It’s a common issue that can occur anywhere in the body, but it is most frequently observed in the neck, back, wrists, and arms.
Understanding the underlying causes of nerve compression is essential to selecting effective treatment options and preventing further nerve damage. Let’s dive deeper into the primary causes of this condition.
Causes of Nerve Compression
Several factors can lead to nerve compression, often stemming from structural or degenerative changes within the body. The primary causes include:
-
Herniated or Bulging Discs: When the soft core of a spinal disc protrudes beyond its outer layer, it can exert pressure on adjacent nerves, leading to conditions like sciatica or cervical radiculopathy.
-
Bone Spurs: Overgrowth of bone, often due to arthritis or degenerative changes, can narrow neural pathways and compress nearby nerves.
-
Spinal Stenosis: A narrowing of the spinal canal, often due to age-related degeneration, can impinge on nerves within the spine.
-
Tendinitis and Repetitive Strain: Repetitive motions may inflame tendons and lead to swelling that compresses nearby nerves, common in the wrists (e.g., carpal tunnel syndrome) or elbows.
-
Tumors and Cysts: Abnormal growths can exert pressure on nerves, although these are less common causes.
-
Trauma or Injury: Fractures, dislocations, or blunt injuries can cause swelling or displaced tissues that compress nerves.
Recognizing what causes nerve compression helps in early diagnosis and targeted intervention.
Symptoms of Nerve Compression
The manifestations of nerve compression depend on its location and severity. Common symptoms include:
- Pain localized near the affected nerve
- Numbness or tingling sensations ("pins and needles")
- Weakness in the muscles served by the compressed nerve
- Burning or sharp sensations
- Reduced reflexes
- Loss of coordination or balance in severe cases
For example, nerve compression in the lower back might cause sciatica, characterized by sharp pain radiating down the leg, while compression in the wrist can result in carpal tunnel syndrome, with numbness in the thumb and fingers.
Diagnosing nerve compression often involves physical examinations, nerve conduction studies, and imaging tests like MRI, which provides detailed views of soft tissues and helps pinpoint the exact cause.
Effective Treatment Options for Nerve Compression
Managing nerve compression requires a tailored approach based on severity and underlying cause. Here are some of the most effective treatment options:
Conservative (Non-Surgical) Treatments
-
Rest and Activity Modification: Reducing activities that aggravate symptoms can prevent worsening of nerve compression.
-
Physical Therapy: Targeted exercises and stretches help relieve pressure, improve flexibility, and strengthen surrounding muscles to support the affected area.
-
Medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain.
- Corticosteroid injections to diminish swelling around the nerve.
- Muscle relaxants in cases of associated muscle spasms.
-
Hot and Cold Therapy: Applying heat or ice packs can help reduce inflammation and alleviate pain.
Interventional Procedures
When conservative treatments fail, clinicians may recommend procedures such as:
- Epidural Steroid Injections: Reduce nerve inflammation and pain.
- Nerve Blocks: Provide temporary relief by blocking nerve signals.
Surgical Interventions
Surgery is considered when pain persists despite conservative measures, or if nerve damage or muscle weakness worsens. Common surgical options include:
- Discectomy: Removal of herniated disc material pressing on nerves.
- Laminectomy: Removal of parts of the vertebrae to widen the spinal canal.
- Carpal Tunnel Release: Cutting the transverse carpal ligament to relieve median nerve pressure.
- Decompression Surgery: Alleviating pressure caused by bone spurs or tumors.
It’s essential to work closely with a healthcare professional to determine the best treatment plan tailored to your specific condition.
Preventing Nerve Compression
Prevention strategies focus on maintaining good posture, performing ergonomic activities, and staying physically active. Here are some tips:
- Practice proper lifting techniques
- Take regular breaks during repetitive tasks
- Maintain healthy weight to reduce strain on the spine
- Incorporate stretching and strengthening exercises into your routine
- Use ergonomic furniture and tools to support proper alignment
A proactive approach can significantly reduce the risk of developing nerve compression and improve overall musculoskeletal health.
Nerve Compression: Key Points at a Glance
- Nerve compression occurs when surrounding tissues exert pressure on a nerve, disrupting normal function.
- Common causes include herniated discs, bone spurs, arthritis, repetitive strain, and traumatic injuries.
- Symptoms often involve pain, numbness, tingling, and muscle weakness.
- Treatment options range from conservative measures like physical therapy to surgical interventions.
- Prevention through posture correction, exercise, and ergonomic practices is vital.
List: Top Activities That May Contribute to Nerve Compression
- Repetitive wrist movements (e.g., typing or using a mouse)
- Heavy lifting without proper form
- Prolonged poor posture, especially while sitting
- Sports injuries involving sudden trauma
- Overuse of certain muscle groups in manual labor
FAQs About Nerve Compression
Q1: What are the early signs of nerve compression I should watch for?
A1: Early signs include persistent tingling, numbness, or mild pain in a specific area, especially after activities involving repetitive movements. Recognizing these symptoms promptly can lead to earlier intervention.
Q2: Can nerve compression heal on its own?
A2: Mild cases may improve with rest, activity modification, and conservative treatments. However, chronic or severe nerve compression often requires medical intervention to prevent permanent nerve damage.
Q3: Is nerve compression only caused by injuries?
A3: No, while injuries can cause nerve compression, degenerative conditions like arthritis, herniated discs, or bone spurs are common contributors as well.
Conclusion: Take Action to Relieve Nerve Compression Today
If you suspect nerve compression is impacting your daily life, don’t wait for symptoms to worsen. Early diagnosis and treatment are key to preventing long-term nerve damage and restoring your comfort and mobility. Consult with a healthcare professional to determine the underlying cause and discuss personalized treatment options. Remember, managing nerve compression effectively starts with awareness—so take action now and regain control of your health and well-being.
For more information, visit trusted sources such as the Mayo Clinic or the National Institute of Neurological Disorders and Stroke. Your journey toward relief begins with understanding and proactive care!