Nerve compression is a common medical condition that can significantly impact your daily life. When a nerve becomes compressed or pinched, it can cause pain, numbness, weakness, and other neurological symptoms. Understanding nerve compression—including its causes, symptoms, and available treatments—can help you seek appropriate care and improve your quality of life. In this article, we’ll break down everything you need to know about nerve compression to empower you to take action.
What Is Nerve Compression?
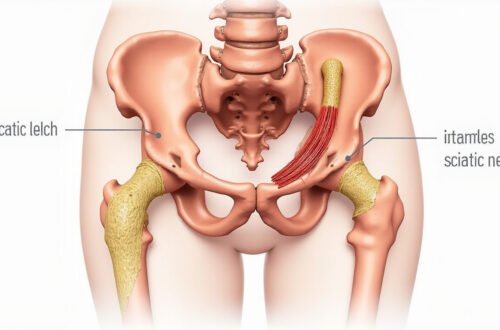
Nerve compression occurs when surrounding tissues, such as bones, cartilage, muscles, or tendons, exert pressure on a nerve. This pressure can disrupt normal nerve function, leading to sensations like pain, tingling, or numbness. The condition can affect any nerve in the body but is most commonly associated with the spine, especially the cervical (neck) and lumbar (lower back) regions.
Understanding nerve compression is crucial because if left untreated, it can lead to permanent nerve damage. Early diagnosis and proper management can prevent complications and reduce discomfort.
Common Causes of Nerve Compression
Nerve compression can result from various underlying factors. Recognizing these causes can help you identify potential risks and seek timely treatment. Here are some of the most common causes:
1. Herniated or Bulging Discs
Discs act as cushions between vertebrae. When a disc herniates or bulges, it can protrude into the spinal canal, pressing on spinal nerves. This is particularly common in the cervical and lumbar spine.
2. Spinal Stenosis
This narrowing of the spinal canal can occur due to aging, arthritis, or congenital conditions. Spinal stenosis puts pressure on the nerves, especially in the lower back and neck.
3. Bone Spurs
Overgrowth of bone, often as a result of osteoarthritis, can form spurs that impinge on nerves.
4. Injuries
Trauma from accidents or falls can cause swelling, fractures, or misalignments that compress nerves.
5. Tumors or Growths
Abnormal growths near nerve pathways can create pressure on nerves.
6. Muscle or Tendon Swelling
Injury or overuse can cause swelling in muscles or tendons, leading to nerve entrapment.
7. Repetitive Movements
Jobs or activities involving repetitive motions can cause nerve impingement over time, such as carpal tunnel syndrome.
Recognizing the Symptoms of Nerve Compression
Symptoms vary depending on the nerve affected and the severity of compression. Early identification can facilitate timely intervention. Here are the most common symptoms:
- Pain: Sharp, burning, or radiating pain along the nerve pathway.
- Numbness or Tingling: Sensations of "pins and needles," especially in extremities.
- Weakness: Loss of strength in muscles served by the compressed nerve.
- Loss of Coordination: Problems with balance or fine motor skills.
- Reflex Changes: Altered reflex responses during neurological exams.
- Muscle Atrophy: Shrinkage or wasting of muscles over time if nerve damage persists.
For example, nerve compression in the cervical spine may cause neck pain radiating into the shoulders and arms, while lumbar nerve compression can lead to sciatic pain down the legs.
Diagnosis of Nerve Compression
Proper diagnosis is essential for effective treatment. Healthcare providers typically perform:
- Physical Examination: Assessing reflexes, muscle strength, and sensory function.
- Imaging Tests: MRI and CT scans visualize soft tissues, discs, and nerves.
- Electrodiagnostic Tests: Nerve conduction studies and EMG measure nerve activity and muscle response.
According to the National Institute of Neurological Disorders and Stroke, early and accurate diagnosis can dramatically improve treatment outcomes (source).
Treatment Options for Nerve Compression
Treatment strategies depend on the underlying cause, severity, and duration of symptoms. Many cases resolve with conservative methods, but some may require surgical intervention.
1. Conservative Treatments
- Rest and Activity Modification: Avoid activities that worsen symptoms.
- Physical Therapy: Exercises to strengthen surrounding muscles, improve posture, and reduce nerve pressure.
- Medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief.
- Corticosteroid injections to decrease inflammation.
- Muscle relaxants if spasms are involved.
- Hot and Cold Therapy: Reduces inflammation and relieves muscle tension.
2. Minimally Invasive Procedures
- Epidural Steroid Injections: Targeted anti-inflammatory injections to relieve nerve swelling.
- Percutaneous Nerve Blocks: Local anesthetic injections to provide temporary relief.
3. Surgical Interventions
When conservative measures fail, surgery may be necessary. Common procedures include:
- Discectomy: Removal of herniated disc material.
- Laminectomy: Removal of part of the vertebral bone to enlarge the spinal canal.
- Foraminotomy: Widening of the nerve root exit passage.
- Spinal Fusion: Stabilizing the spine after decompression.
Note: Surgical options should be discussed thoroughly with a spine specialist or neurosurgeon to weigh benefits and risks.
Preventing Nerve Compression
Preventive measures are key to avoiding nerve compression. These include:
- Maintaining good posture, especially when sitting or working at computers.
- Regularly participating in physical activity to strengthen core muscles.
- Using ergonomically designed furniture and tools.
- Avoiding repetitive motions or taking frequent breaks.
- Managing weight to reduce undue stress on the spine.
- Staying aware of symptoms and seeking early medical advice.
Bullet List: Tips for Managing Nerve Compression at Home
- Apply ice or heat packs as needed for pain relief.
- Engage in gentle stretching exercises recommended by your healthcare provider.
- Practice good ergonomics at your workstation.
- Keep active within pain limits to promote circulation and healing.
- Maintain a healthy weight to lessen spinal and nerve stress.
Frequently Asked Questions About Nerve Compression
1. What are the early signs of nerve compression?
Early signs include mild pain, tingling sensations, or numbness in the affected area. Recognizing these symptoms early can lead to more effective treatment and prevent long-term damage.
2. Can nerve compression go away on its own?
Mild cases of nerve compression often improve with conservative treatments such as rest, physical therapy, and medication. However, persistent or severe symptoms should be evaluated by a healthcare professional to prevent permanent nerve damage.
3. How is nerve compression diagnosed?
Diagnosis involves a physical exam, imaging tests like MRI or CT scans, and neurological assessments to pinpoint the source and severity of compression.
The Importance of Seeking Professional Care
If you experience symptoms like persistent pain, numbness, weakness, or tingling, consulting a healthcare professional is vital. Early diagnosis and management can prevent complications, improve outcomes, and restore your daily function.
Take Action Today to Relieve Nerve Compression
Understanding nerve compression and its treatment options empowers you to take control of your health. If you’re experiencing symptoms suggestive of nerve impingement, don’t wait—seek medical advice promptly. Modern treatments offer effective relief through non-invasive methods or surgical options when necessary. Prioritize your neurological health today, and connect with a qualified healthcare provider to develop a personalized treatment plan. Your journey to pain relief and improved mobility starts now.
References: